For the first time in history, the entire human race is confronted with a single common enemy – the virus causing COVID-19. Even as the virus is spreading disaster on an unprecedented scale, a race is on to build a vaccine that will save us. This month’s column takes a peek into the fascinating world of vaccines.
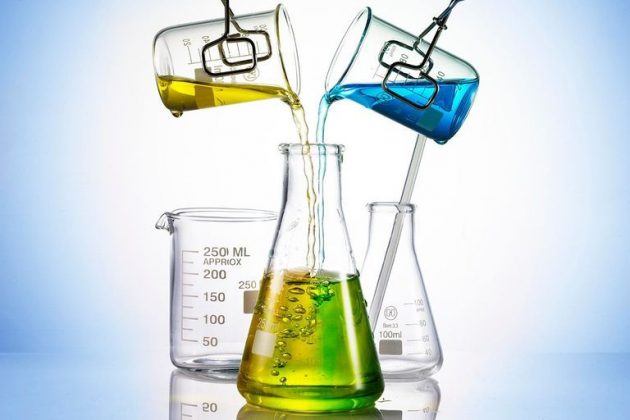
With COVID-19 spreading fear and death across the globe, many medical professionals are of the opinion that only a vaccine can be the silver bullet against this scourge. Vaccines are biological preparations of antigens, the proteins found on the surface of pathogens. Antigens alert our body to the infection and trigger an immune response. The world of vaccines is fascinating with many principles of chemistry and chemical engineering
at play.
Classical Vaccines
Vaccines come in many types. Classical vaccines use the entire microbe, either weakened or dead. The earliest vaccines used live virus or bacteria that have been deliberately weakened. Famous examples include the smallpox vaccine of Edward Jenner and the rabies vaccine of Louis Pasteur. These attenuated vaccines evoke a strong immune response and confer lifelong immunity after just one or two doses. Attenuated vaccines are easy to produce for certain classes of viruses, but difficult for others. Inactivated vaccines use dead bacteria or virus, as in the case of polio. The microbe is killed by chemicals, heat or radiation. Toxoid vaccines use diluted dosages of the toxins produced by the invading
bugs. Best examples of this category are diphtheria and tetanus vaccines. The discovery of the toxoiding process for the diphtheria vaccine was a stroke of serendipity; the residual formalin after cleaning of containers was found to have weakened the toxin.
Modern Vaccines
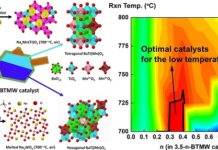
Sub-unit vaccines use only part of a target pathogen to provoke a response from the immune system. This may be done by isolating a specific protein from a pathogen and presenting it as an antigen on its own. Including only the essential antigens in a vaccine can minimise side effects. Conjugate vaccines consist of 2 components – the antigen and a carrier protein – linked covalently, and elicit a very powerful immune response. They are central to all infant immunisations. Another kind of subunit vaccine, called recombinant vaccine, is created by genetic engineering. It involves inserting the DNA from the virus into another cell to make them produce the active ingredient, a protein, for the vaccine. This technique was successfully used to produce a vaccine against Hepatitis B.
Manufacturing Process
Viral vaccines are manufactured by growing mammalian or avian host cells in a controlled environment and infecting them with the target virus. The manufacturing process has 3 steps – growth, harvesting and purification. A typical process begins with growing the cell culture by fermentation in a series of bioreactors. The raw materials have to be identical for every batch – a certified vial of the culture from a seed bank. Once the cells have increased 5-10 fold in the seed reactor, they are transferred to the production reactor where they increase by another 5-10 times. There is a series of fermentors, each 5-10 times bigger than the previous one. By the time the cellgrowth phase ends, the cells would have increased thousands of times. The microbes can be fussy about the nutrients and the medium. The process demands precise control and absolute sterility. In the final growth step the cells are infected with the genetically modified virus. The active vaccine intermediate is harvested from the growth media by dead-end or crossflow filtration, or centrifuging. The main process parameters for control and optimisation are pH, dissolved oxygen concentration, cell concentration at infection, quantity of virus inoculated per cell at infection, medium composition, and timing of harvest. The manufacturing facility should be GMP compliant and should have adequate containment level, usually BSL-2.
Purification
Purification is a key step in vaccine production for getting regulatory approvals. Vaccines should be free of all contaminants that can provoke adverse reactions in the recipients. Purification has 3 stages. The first step is to quickly isolate the target molecule from conditions that could lead to its inactivation or loss. The second step is to eliminate the contaminants. The final polishing step removes trace impurities. Various solid-liquid separation techniques, like filtration, centrifuging, chromatography are widely used in the purification process. Chromatography is a very powerful technique for the polishing step because the impurities have similar characteristics as the target molecule. New chromatographic resins with multimodal binding ligands have simplified the purification steps. Membrane chromatography is also an attractive option. The chromatographic processing of vaccines continues to evolve with a focus on reducing the number of steps and improving the yield.
Formulation
Formulation and filling of vaccines pose many technological challenges. Formulation is usually dilution of a high potency bulk product to the appropriate strength. As vaccines volved they got safer, but at the cost of efficacy. This loss of efficacy is compensated by adding adjuvants. Adjuvants make the vaccines work better by evoking stronger immune response from the recipients. Aluminium salts, such as aluminium hydroxide, aluminium phosphate, and aluminium potassium sulphate have been used safely as adjuvants for more than 70 years. Antigens are adsorbed on the aluminium adjuvants and it is important to ensure homogeneity during the formulation and filling process. Stabilisers are added to maintain the vaccine’s effectiveness during storage, particularly where the cold chain is unreliable. The quality expectations of a vaccine are stringent because it will be administered to millions of perfectly healthy people. Even leachates from glass vials and their rubber stoppers are a matter of concern.
Nucleic Acid Vaccines
Recently, a radically new approach to vaccination has been developed. It involves the direct
introduction of the DNA or RNA sequence encoding the antigen against which an immune response is sought. By in situ production of the target antigen, our bodies become vaccine factories. Nucleic Acid vaccines are non-viral vaccines and have a number of potential advantages – stimulation of improved immune responses, improved vaccine stability, the
absence of any infectious agent and the relative ease of large-scale manufacture. The production process avoids the use of problematic starting materials such as animal- derived components, and results in high batch-to-batch reproducibility.
Production Platforms
Furthermore, the same production process can be used for many different vaccines. This platform characteristic of the production process eliminates several expensive steps required to fulfil regulatory demands. The process can be easily adapted to GMP conditions and the time between clinical trials and commercial production can be significantly shortened. The total production process is highly flexible and scalable; it can be easily changed to the production of a new vaccine within a few days. Also, the process can be scaled to the production of millions of vaccine doses either in one big facility or in several smaller ones. While many clinical trials of these new age vaccines are underway, none of them have been licensed so far.
Epilogue
Even as this is being written (19th March), the first Phase-I clinical trial for mRNA vaccine, a type of nucleic acid vaccine, against COVID-19 is underway in USA. The biotech company, Moderna, was already researching the coronavirus behind the Middle East Respiratory Syndrome (MERS) and was thus able to adapt their methodology and vaccine design towards SARS-CoV-2, the virus responsible for COVID-19.
Two other German biotech companies – CureVac and BioNTech – are also in the race to develop a mRNA vaccine against COVID-19. Hopefully one of them would be the silver bullet that humanity is in desperate need now..
Readers’ responses may be sent to:
k.sahasranaman@gmail.com or
chemindigest@gmail.com